What is a Clinical Audit?
A Clinical Audit, formerly known as a Medical Audit, aims to improve the quality of patient care and clinical outcomes through the peer-led review of practice against evidence-based standards. As a quality improvement process, local and national clinical audits can help healthcare practitioners identify deficits in current practice, administer excellent clinical service, and uphold professional standards.
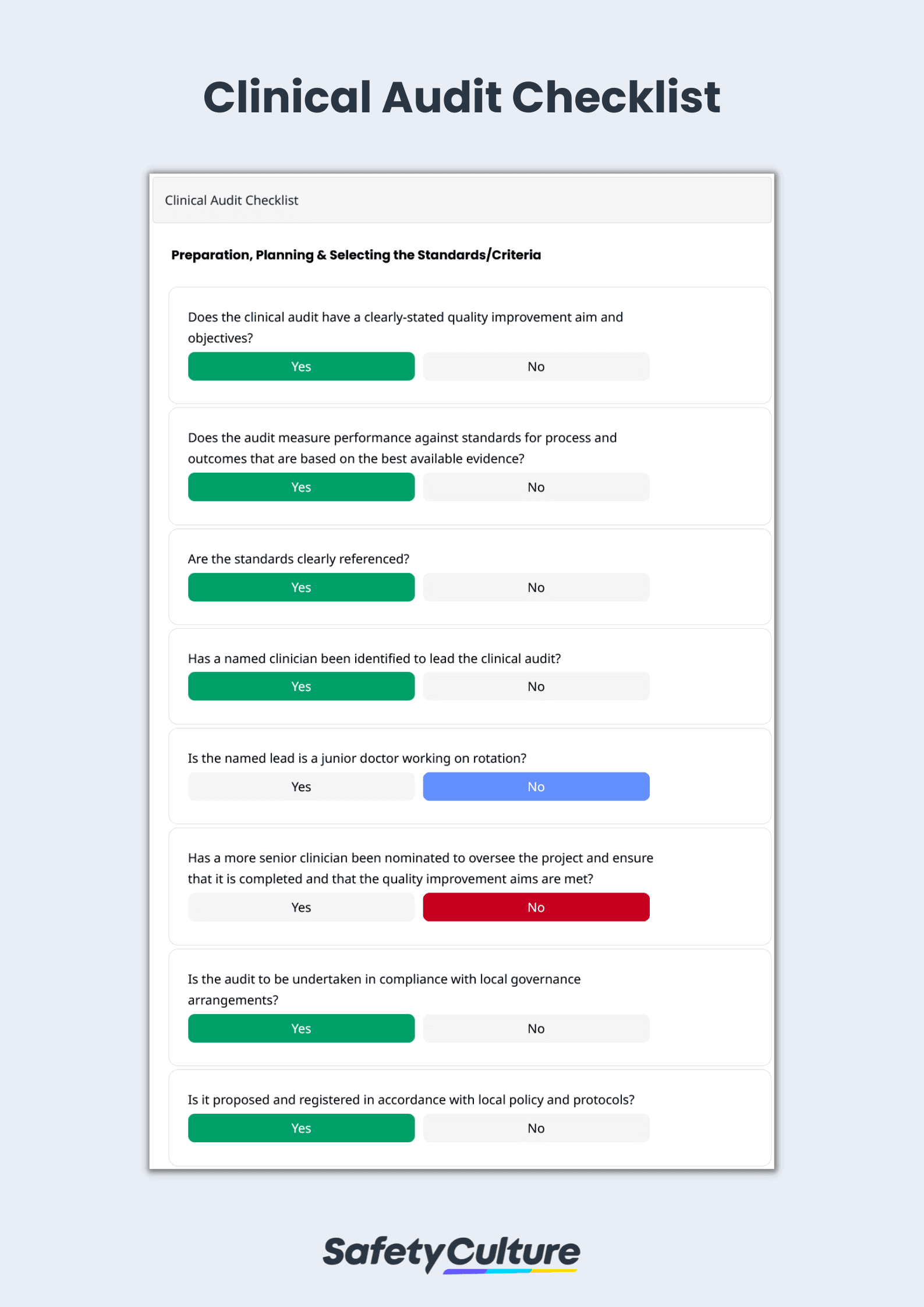
Multidisciplinary teams in healthcare facilities use a clinical audit checklist to ensure the completion of the clinical audit cycle—preparation and planning, selecting the standards/criteria, measuring performance, implementing changes, and sustaining improvements.
Crucial Areas of Patient Care
Preparation and planning for the clinical audit begin by determining exactly what the multidisciplinary team (clinical audit committee) should be auditing. As a rule of thumb, an area of care where obvious shortcomings exist is the starting point of clinical audits. Clinical improvement managers and audit leads should also look at high-volume, high-risk, and high-cost areas such as the following:
Intensive/Critical Care Unit
High-risk sepsis admissions from the ward, unit-acquired infections in the blood, and out-of-hours discharges to the ward have significantly decreased in different parts of the UK as a result of clinical audits. To prevent avoidable infection during patient care, the clinical audit committee should regularly assess the hand hygiene techniques of healthcare practitioners using a mobile-ready hand hygiene audit checklist. After 3-6 months of implementing changes, a clinical re-audit is necessary to validate the effectiveness and sustain improvements.
Medical Records
Quality healthcare is based on accurate and complete clinical documentation in medical records. US healthcare institutions and their associates who handle protected health information should stay compliant with the Health Insurance Portability and Accountability Act (HIPAA) by conducting security risk assessments. The clinical audit committee should evaluate the administrative, physical, and technical safeguards currently in place, address time-sensitive gaps, and avoid costly fines and legal action with a digitized HIPAA compliance and medical checklist, along with SOAP notes for various applications (e.g., occupational therapy).
Admission and Discharge
Non-clinical transfers, unplanned readmissions, and delayed discharges result in low patient satisfaction. The clinical audit committee should inspect transitions of care, medication safety, and outpatient follow-up procedures to reduce bottlenecks and ease patient flow. Starting discharge planning on the date of admission and writing digital SOAP notes, instead of hiring medical scribes, also shortens wait times and encourages more patient-centered care. Common clinical audit improvements include new documentation methods, better communication systems, and efficient checking mechanisms.
Clinical Audit Example
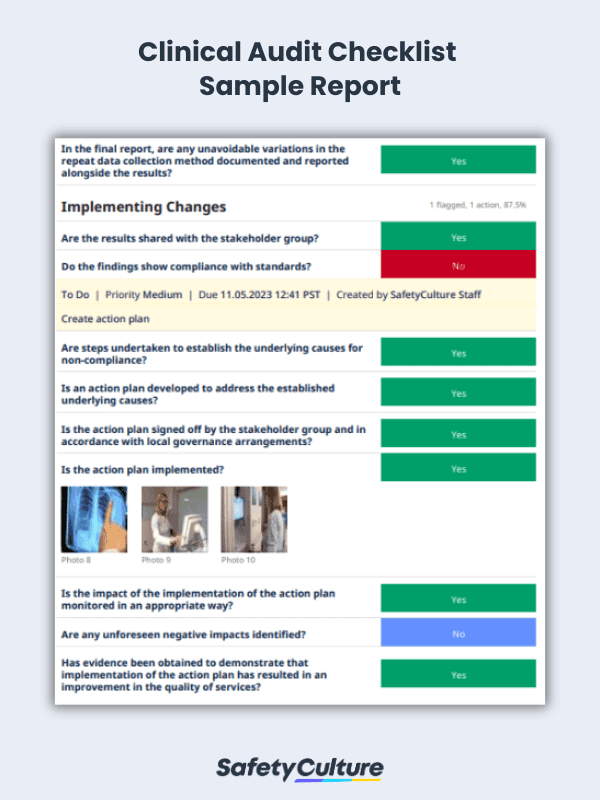
Conduct clinical audits to provide the best care for the patients in the healthcare facility. This practice will ease process review, recordkeeping, and that necessary corrective action will be followed through. View this sample clinical audit PDF and here’s an example of a clinical audit report: